- The coronavirus pandemic has infected nearly 14 million people in a matter of months, and scientists are racing to develop a vaccine at record speed.
- But vaccines often take years, and sometimes even decades, to develop, test, and approve for public use.
- To gain some perspective on what researchers developing a coronavirus vaccine are up against, here’s how long it took to develop vaccines for other infectious diseases throughout history.
- Visit Business Insider’s homepage for more stories.
Across the world, scientists have been working at record speed to develop a successful vaccine for the novel coronavirus, which has already infected more than 13 million people and killed at least 593,000 worldwide.
With no known cure or treatment in sight, many believe a vaccine is the most ideal option to prevent future outbreaks of the virus – but vaccines can take years, and sometimes even decades, to be developed.
In the US, vaccine development undergoes a specific set of steps that includes exploratory phases, pre-clinical trials, new drug application, four phases of vaccine trials, and thorough vetting from the US Centers of Disease Control and Prevention and the Food and Drug Administration.
All of that combined could take multiple years, and even then, it might not be as effective as hoped.
"I would be extremely happy to be wrong, but I don't really see how a vaccine can get put together in time to help out with the likely course of this current outbreak," Derek Lowe, author of the industry blog In The Pipeline who has more than 30 years of experience in drug discovery, told Business Insider's Andrew Dunn.
But because of the severity of the pandemic, manufacturers and leading scientists have made efforts to shift funding and expedite the process to yield results as quickly as possible.
Dr. Anthony Fauci, the US government's top infectious-disease expert, has previously testified in front of Congress that a vaccine could be developed by the end of this year, or available for use in 2021.
But it's too soon to tell. While some drug companies have entered trial stages and shown positive results, there is still no guarantee a working vaccine will ever be developed for COVID-19.
To gain some perspective on the complexities of vaccine development, here's how long it took to develop vaccines for other infectious diseases throughout history.
Smallpox

The eradication of smallpox through a vaccine is seen as one of the biggest achievements in public health history - but it took several centuries to get there.
The origins of smallpox is unknown, though scientists believe it dates all the way back to the Egyptian Empire of the 3rd Century BCE. By the 18th century, colonization spread the disease across the globe. It had a devastating mortality rate of up to 30%.
In 1796, Edward Jenner in the UK created the first successful smallpox vaccine, but it wasn't until the 1950s that vaccine treatments began to effectively eradicate the disease in some parts of the world.
Then, in 1967, a global effort that provided a higher level of vaccine production and an advancement in needle technology eventually lead to eradication of the disease by 1980.
To date, smallpox remains the only disease to have been completely eliminated around the world through vaccination efforts.
Plague
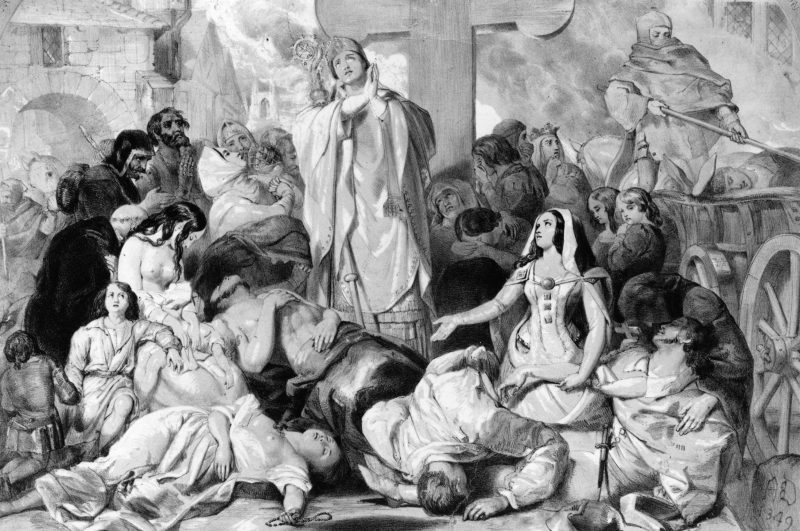
Plague is one of the world's oldest and most lethal diseases, culminating in nearly 200 million deaths throughout human history. But to date, no licensed vaccine is available.
Plague is perhaps most notorious for killing millions of people during the Middle Ages, but the disease is still active in areas around the world. As recent as 2017, a plague outbreak in Madagascar attracted widespread attention and panic.
However, since plague is a disease spread by bacteria, the advent of modern antibiotics can be used as treatment. Even so, researchers believe that vaccination development is the most viable option to prevent the spread of disease in the long-term.
Many failed attempts have been made to create a plague vaccine in the past - including one that was made in the US to inoculate soldiers during the Vietnam War.
But in 2018, the WHO created a Plague Vaccine Target Product Profile, which lists off 17 possible candidates for vaccine approval, which are undergoing clinical trials and moving toward FDA approval.
Typhoid Fever

Typhoid fever is a deadly disease that can be spread widely through food and water. Though relatively uncommon in industrialized areas, it remains a significant threat in developing nations throughout Southeast Asia, Africa, and Latin America.
Two vaccines are commercially available to prevent typhoid fever. After the bacteria responsible for the disease was discovered in 1880, German scientists first began research into these efforts in 1896.
In 1909, US Army physician Frederick F. Russell developed the first US typhoid vaccination. For the next several years, the vaccine would be used for military purposes, but in 1914, it became available among the general American public.
Today, Typhoid fever is uncommon in the US and vaccinations are not commonly recommended for routine use.
Yellow Fever

In 1951, Max Theiler became the first and only scientist to receive a Nobel Prize for the development of a vaccine. His efforts to control yellow fever are widely praised by the scientific community, and he helped to correct years of misled research.
Yellow fever has caused deadly epidemics throughout human history for more than 500 years, and by the end of the 19th century, it was well known to be a threat around the world. But little was known about the disease itself, and early vaccination efforts at the close of the century mistakenly focused on bacterial transmission when it's actually caused by a virus.
In 1918, researchers working for the Rockefeller Institute developed what they thought was the first successful yellow fever vaccination - but in 1926 Theiler proved otherwise and the faulty vaccine ceased production.
Over a decade later, in 1937, Theiler created the first safe and effective yellow fever vaccination, which has since become the universal standard.
Influenza

Influenza has a long, tragic history of killing millions of people worldwide. During the 1918 influenza pandemic, there were no known cures or vaccinations for the virus.
Starting in the 1930s, it took decades of research to understand the complexities of the influenza virus, and it wasn't until 1945 that the first vaccine was approved for use in the US.
But just two years later, in 1947, researchers concluded that seasonal changes in the composition of the virus rendered existing vaccinations ineffective.
Researchers realized that two main types of influenza viruses occur - influenza A and influenza B, along with multiple new strains of the virus each year. Because of this, scientists have to tweak the influenza vaccine every year.
Today, seasonal flu vaccines are designed by the WHO using data gathered from influenza surveillance centers to develop a new vaccination based off the three strains most likely to circulate in the upcoming season.
Polio

While polio has likely affected human populations for thousands of years, it wasn't until the late 1800s that the disease reached epidemic proportions. At the turn of the century, polio tore through the US, leaving many infected patients paralyzed or disabled for life.
Research to understand polio was gradual for the first few decades of the 20th century. In 1935, a vaccination was attempted, first on monkeys and then on children in California. Though this vaccine yielded poor results, two more decades of research paved the way for the development of vaccines by Jonas Salk in 1953, and Albert Sabin in 1956.
After a trial of more than 1.6 million children, Salk's vaccine was adopted in the US by 1955. Continuous research through the 1980s made way for an even more effective and efficient production of vaccines, and by 1994 polio was eliminated in the Americas.
As recently as 1988, 350,000 people had the debilitating disease, the majority of whom were children. By 2018, there were only 33 cases of polio in the whole world.
Last year saw a slight uptick in the number of cases, with 544. Once we get that number to zero, polio would become only the second human disease we've ever wiped from the planet.
Anthrax

Anthrax is thought to have been around since 700 BC, but the first clinical account of the disease was recorded in the 1700s.
Throughout the 1800s, a series of studies to determine where the disease originated from, how long the bacteria could survive, and how the disease transmitted through animals paved the way for the first attempts at a vaccine in 1881.
In 1937, scientist Max Sterne created a successful Anthrax vaccination to be used in livestock, a version of which is still used today, in order to reduce transmission from animals to humans. Thirteen years later, the first human vaccine was created and made available for people working in animal processing mills in the United States.
An updated anthrax vaccine was developed in 1970, which is largely what's used to prevent the disease in humans today.
Measles, Mumps, and Rubella (MMR)

Measles, Mumps, and Rubella are viral infections that have each caused widespread, deadly disease outbreaks. Throughout the 1960s, individual vaccines were developed for each of them, but a decade later, they were combined into one.
Measles was the first of the three to receive its own vaccine in 1963, followed by mumps in 1967, and rubella in 1969. Two years later, in 1971, Maurice Hilleman of the Merck Institute of Therapeutic Research developed a combined vaccination that would provide immunity for all three viruses.
Hilleman was credited with creating the first measles and mumps vaccine, and began researching ways to incorporate a system of immunity for each virus. Using his previous research and a rubella vaccine developed by Stanley Plotkin in 1969, he created the first successful MMR vaccine in just two years.
According to the CDC, "One dose of MMR vaccine is 93% effective against measles, 78% effective against mumps, and 97% effective against rubella."
"Two doses of MMR vaccine are 97% effective against measles and 88% effective against mumps."
Varicella (Chicken Pox)

Primary varicella infection, commonly known as chickenpox, was misdiagnosed as smallpox until the end of the 1800s. In the 1950s, scientists distinguished varicella from herpes zoster (shingles), and subsequent research lead to the development of first vaccine for chickenpox in Japan in the 1970s.
The vaccine was licensed for use in the US in 1995.
Shingles (herpes zoster)

Shingles, or herpes zoster, stems from the same virus that causes chickenpox. The only two ways shingles can develop is after an intital infection of chickenpox, or (uncommonly) exposure to a chickenpox vaccination.
The connection between shingles and chickenpox was first observed in 1953, and throughout the 1960s, studies indicated that shingles was much more common in older populations. But it wasn't until 2006 that the first commercially available vaccine was licensed in the US.
A more recent licensed vaccine for shingles came with a recommendation by the US Advisory Committee on Immunization Practices in 2018 that adults age 60 or older should be vaccinated for the disease.
Hepatitis B

Hepatitis B is a more recent virus, and was discovered by Dr. Baruch Blumberg in 1965. Just four years later, he created the first hepatitis B vaccine using a heat-treated form of the virus.
Twelve years later, in 1981, the FDA approved of the first commercially available hepatitis B vaccination, which involved blood samples from infected donors.
Then, in 1986, a new synthetically prepared vaccine that does not use blood products replaced the original model.
Since Hepatitis B can cause liver cancer, the vaccine was also considered the first anti-cancer vaccine.
Human papillomavirus (HPV)

Human papillomavirus (HPV) is the most commonly sexually transmitted disease in the US, and studies show that more than 80% of women will have contracted the virus at some point in their lives.
Two strains of HPV are thought to cause up to 70% of cervical cancer, which can result in hundreds of thousands of deaths each year. The link between HPV and cervical cancer was first made in 1981, and over two decades of research followed before a viable vaccine hit the market.
The first HPV vaccine was developed in the US in 2006, and subsequent research has lead to the development of two more vaccines since.
Today, recommendations on what type of vaccine to get largely depends on age.
