- The coronavirus pandemic is causing economic pain for many US hospitals.
- New data shows 21% of doctors are facing pay cuts or furloughs as health systems try to reduce costs.
- A smaller percentage say they’re considering leaving medicine all together, which could deal a further blow to America’s ongoing shortage of physicians.
- Visit Business Insider’s homepage for more stories.
An increasing number doctors are facing furloughs and pay cuts, to the point some are even considering changing jobs, as the coronavirus pandemic strains many hospitals’ finances.
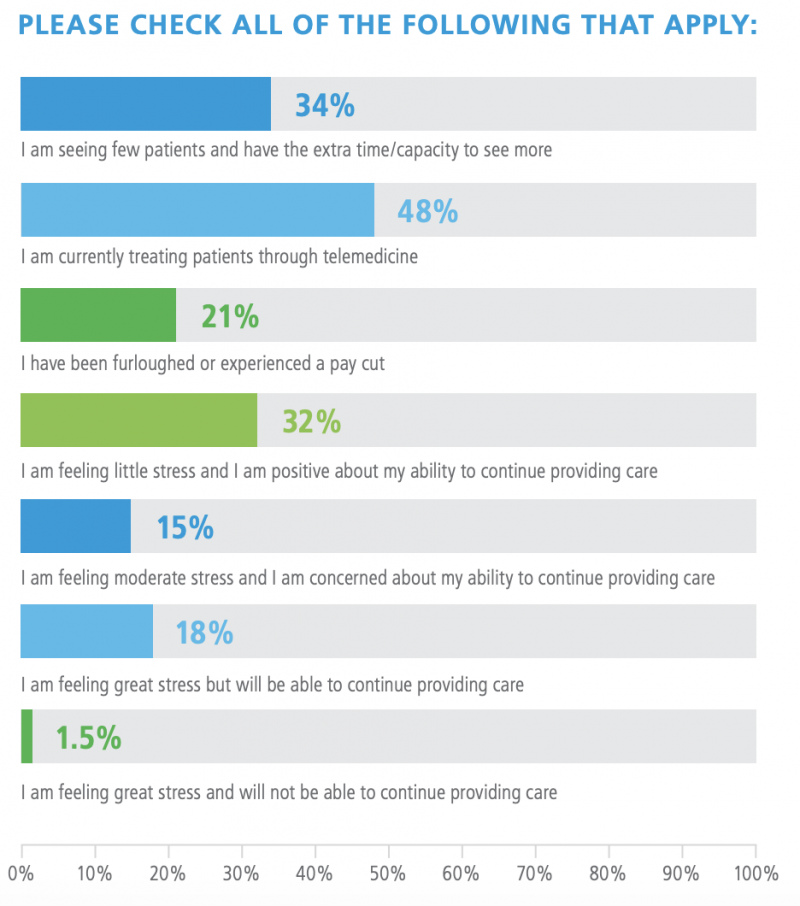
A fifth of the 842 physicians, 21%, surveyed by the physician recruitment firm Merritt Hawkins said they’ve experienced pay cuts or have been furloughed as a result of the crisis. More doctors who aren’t actively treating COVID-19 cases say they’ve experiencing the effects of cost-cutting than those who are, but even those on the front line were not immune to the economic impact.
Physicians aren’t alone. Federal data for March showed some of the largest employment declines in the record uptick in unemployment happened in the outpatient sector.
Across the country, hospitals’ balance sheets have been hit hard by the pandemic. For non-COVID care, the normal routines of medicine have been radically shifted. Doctor visits have moved largely online – a trend confirmed by Merritt’s survey – while stay-at-home orders result in fewer emergency visits from accidents, while other elective surgeries are postponed. The overall reduction has hurt revenue that hospitals rely on.
According to Business Insider's Kimberly Leonard, there's no complete tabulation anywhere of the cuts made by hospitals. However, The American Hospital Association, which represents more than 5,000 hospitals, has sounded the alarm about the industry's financial difficulties and said that quickly distributing funding from the CARES Act would help facilities keep their doors open.
As part of that aid package, some $100 billion is set aside for hospitals, with even more funding included in another round of economic aid signed into law by President Donald Trump on Friday.
But some doctors aren't waiting around for the help.
As a result of the pandemic, 14% of physicians said they plan to seek a different practice, and 6% said they planned to exit patient care entirely.
"Prior to the pandemic, physicians were already facing a number of stress factors eroding their morale and potentially limiting patient access to their services," the study concluded. "These trends were of concern prior to the pandemic due to the growing shortage of physicians nationwide. The coronavirus is likely to add to these stresses, and more attention therefore needs to be paid to physician well-being, both during the current crisis and after it has been contained, to help ensure an adequate and engaged physician workforce."
Travis Singleton, executive vice president of the firm behind the survey, said the results show a clear need for more physicians.
"The overall answer, and this was true before the pandemic and after, is we need more physicians," he told the Dallas Business Journal.
"That won't be solved until we increase the U.S. residency slots. What else can you do? You have everyone practice to the limits of their CV. Increase use of nonphysician clinicians. Nurse practitioners, physician assistants, nursing case managers, care team environments."

